 “Our study shows that muscle stem cells are primed to start muscle repair right away, but the immune cells maintain the stem cells in a resting state while they finish the cleanup job." - Dr. Jeffrey DilworthA new study published in the journal Science reveals a unique form of cell communication that controls muscle repair. In damaged muscle, stem cells must work together with immune cells to complete the repair process, yet how these cells coordinate to ensure the efficient removal of dead tissue before making new muscle fibers has remained unknown. The scientists have now shown that a natural substance called hyaluronic acid, which is used in cosmetics and injections for osteoarthritis, is the key molecule that manages this fundamental interaction.
“Our study shows that muscle stem cells are primed to start muscle repair right away, but the immune cells maintain the stem cells in a resting state while they finish the cleanup job." - Dr. Jeffrey DilworthA new study published in the journal Science reveals a unique form of cell communication that controls muscle repair. In damaged muscle, stem cells must work together with immune cells to complete the repair process, yet how these cells coordinate to ensure the efficient removal of dead tissue before making new muscle fibers has remained unknown. The scientists have now shown that a natural substance called hyaluronic acid, which is used in cosmetics and injections for osteoarthritis, is the key molecule that manages this fundamental interaction.
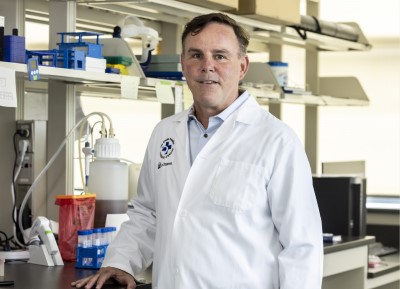
“When muscles get damaged, it is important for immune cells to quickly enter the tissue and remove the damage before stem cells begin repair,” said Dr. Jeffrey Dilworth, senior scientist at The Ottawa Hospital and professor at the University of Ottawa and senior author on the study. “Our study shows that muscle stem cells are primed to start repair right away, but the immune cells maintain the stem cells in a resting state while they finish the cleanup job. After about 40 hours, once the cleanup job is finished, an internal alarm goes off in the muscle stem cells that allows them to wake up and start repair.”
 “If we could find a way to enhance hyaluronic acid production in the muscle stem cells of older people it might help with muscle repair.”- Dr. Kiran NakkaDr. Dilworth and his team identified hyaluronic acid as the key ingredient in this internal alarm clock that tells muscle stem cells when to wake up. When muscle damage occurs, stem cells start producing and coating themselves with hyaluronic acid. Once the coating gets thick enough, it blocks the sleep signal from the immune cells and causes the muscle stem cells to wake up.
“If we could find a way to enhance hyaluronic acid production in the muscle stem cells of older people it might help with muscle repair.”- Dr. Kiran NakkaDr. Dilworth and his team identified hyaluronic acid as the key ingredient in this internal alarm clock that tells muscle stem cells when to wake up. When muscle damage occurs, stem cells start producing and coating themselves with hyaluronic acid. Once the coating gets thick enough, it blocks the sleep signal from the immune cells and causes the muscle stem cells to wake up.
Using mouse and human tissues, Dr. Dilworth and his team also discovered how muscle stem cells control the production of hyaluronic acid using epigenetic marks on the Has2 gene.
“Interestingly, aging is associated with chronic inflammation, muscle weakness and a reduced ability of muscle stem cells to wake up and repair damage,” said lead author Dr. Kiran Nakka, a research associate with Dr. Dilworth who conducted this research as part of his postdoctoral studies. “If we could find a way to enhance hyaluronic acid production in the muscle stem cells of older people it might help with muscle repair.”
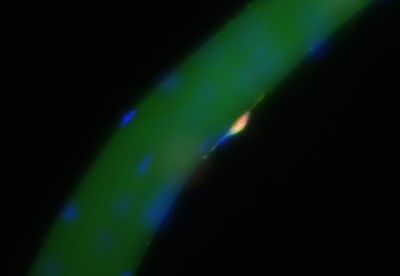 When a muscle fiber is damaged, stem cells (in pink) start producing and coating themselves with hyaluronic acid (pale green outline). Once the coating gets thick enough, it causes the muscle stem cells to wake up.The authors note that the regenerative effect of hyaluronic acid seems to depend on it being produced by the muscle stem cells. The team is currently examining if drugs that modify the epigenetics of muscle stem cells could be used to increase their production of hyaluronic acid.
When a muscle fiber is damaged, stem cells (in pink) start producing and coating themselves with hyaluronic acid (pale green outline). Once the coating gets thick enough, it causes the muscle stem cells to wake up.The authors note that the regenerative effect of hyaluronic acid seems to depend on it being produced by the muscle stem cells. The team is currently examining if drugs that modify the epigenetics of muscle stem cells could be used to increase their production of hyaluronic acid.
About Dr. Dilworth: Dr. Jeffrey Dilworth is a senior scientist in the Regenerative Medicine Program at The Ottawa Hospital, which includes the Sprott Centre for Stem Cell Research and the Sinclair Centre for Regenerative Medicine. He is also a Professor in the Department of Cellular and Molecular Medicine at the University of Ottawa, with a cross-appointment to the Departments of Medicine and Surgery. Dr. Dilworth is also the Director of the Ottawa Centre for Epigenetics Research, a member of the Stem Cell Network, and recipient of The Ottawa Hospital’s Chrétien Researcher of the Year Award for 2021. Dr. Dilworth and the other authors of this paper declare that they have no competing interests.
Full reference: JMJD3 activated hyaluronan synthesis drives muscle regeneration in an inflammatory environment. Kiran Nakka, Sarah Hachmer, Zeinab Mokhtari, Radmila Kovac, Hina Bandukwala, Clara Bernard, Yuefeng Li, Guojia Xie, Chengyu Liu, Magid Fallahi, Lynn A. Megeney, Julien Gondin, Bénédicte Chazaud, Marjorie Brand, Xiaohui Zha, Kai Ge, F. Jeffrey Dilworth. Science. August 4, 2022.
Funding and support: This research was funded by the Canadian Institutes of Health Research and the National Institutes of Health. All research at The Ottawa Hospital is also enabled by generous donors to The Ottawa Hospital Foundation. Core resources used in this research include StemCore, Flow Cytometry and Cell Sorting, Cell Biology and Image Acquisition.
About The Ottawa Hospital: The Ottawa Hospital is one of Canada’s top learning and research hospitals, where excellent care is inspired by research and driven by compassion. As the third-largest employer in Ottawa, our support staff, researchers, nurses, physicians, and volunteers never stop seeking solutions to the most complex health-care challenges. Our multi-campus hospital, affiliated with the University of Ottawa, attracts some of the most influential scientific minds from around the world. Backed by generous support from the community, we are committed to providing the world-class, compassionate care we would want for our loved ones. www.ohri.ca
About the University of Ottawa: The University of Ottawa is home to over 50,000 students, faculty and staff, who live, work and study in both French and English. Our campus is a crossroads of cultures and ideas, where bold minds come together to inspire game-changing ideas. We are one of Canada’s top 10 research universities—our professors and researchers explore new approaches to today’s challenges. One of a handful of Canadian universities ranked among the top 200 in the world, we attract exceptional thinkers and welcome diverse perspectives from across the globe. www.uottawa.ca
Media contact:
Amelia Buchanan
Senior Communication Specialist
Ottawa Hospital Research Institute
613-297-8315
ambuchanan@ohri.ca
