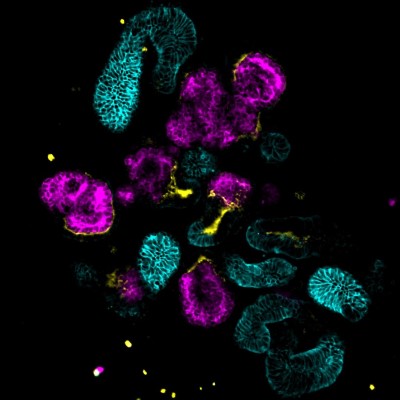
 Microscope image of genetically engineered kidney organoids that were used to solve a medical mystery about tuberous sclerosis complex. Image Credit: Cell ReportsResearchers have solved a medical mystery in a poorly understood disease by uncovering which cells cause tumours in patients with tuberous sclerosis complex (TSC). As described in Cell Reports, they did this by creating genetically engineered kidney organoids, or “mini-kidneys” grown from human tissue.
Microscope image of genetically engineered kidney organoids that were used to solve a medical mystery about tuberous sclerosis complex. Image Credit: Cell ReportsResearchers have solved a medical mystery in a poorly understood disease by uncovering which cells cause tumours in patients with tuberous sclerosis complex (TSC). As described in Cell Reports, they did this by creating genetically engineered kidney organoids, or “mini-kidneys” grown from human tissue.
“The cells at the origin of tuberous sclerosis tumours have been a mystery for decades,” said senior author Dr. Bill Stanford, senior scientist at The Ottawa Hospital and professor at the University of Ottawa. “Our results can help find possible treatment targets for this challenging disease.”
TSC is a rare genetic disease that causes benign tumours in the skin, brain, kidneys, heart or lungs. TSC tumours are very diverse, arising in children or adults with a range of symptoms from mild to life-threatening and often include seizures and kidney problems. There is no cure and treatment options are limited.
“Kidney disease is the leading cause of death in patients with TSC. Around 60 to 80 percent of patients develop tumours in their kidneys, often reducing kidney function and sometimes leading to catastrophic bleeding,” said lead Dr. Adam Pietrobon, MD-PhD student at The Ottawa Hospital and the University of Ottawa. “There were no adequate lab models to study how TSC affects the kidney, so we made one ourselves.”
TSC is caused by mutations in the TSC1 or TSC2 gene. For most patients, these mutations arise spontaneously during development or early life rather than being inherited from their parents. This makes TSC a difficult disease to study. While lab researchers often use animals to study human diseases, there was no animal model that fully captured TSC’s impact on the kidneys.
TSC tumours in the kidney have puzzled experts because they are extraordinarily diverse in size, cellular makeup and gene expression, even within the same patient. What causes this diversity was unknown, and it makes treatment challenging.
To better understand the impact of TSCs on the kidneys, the team grew 3D kidney tissue in the lab from human stem cells that were genetically engineered to have a TSC1 or TSC2 mutation. Known as organoids, these miniature, simplified versions of kidneys had a genetic profile similar to TSC tumours found in patents. The researchers then took single cells from these kidney organoids and injected them into the kidneys of mice, where they grew into human TSC tumours.
Using these organoids, the researchers revealed that cells called Schwann Cell Precursors are where TSC tumours start in the kidney. They also found this single mutation affects the development of many different kinds of cells, which explains the variation in kidney tumours even within the same person.
“Not only can these ‘mini-kidneys’ help us to better understand this disease, they can also be used to test new therapies,” said Dr. Pietrobon.
Authors: Adam Pietrobon, Julien Yockell-Lelièvre, Trevor A. Flood, William L. Stanford
Core resources: Human Pluripotent Stem Cell Facility, StemCore, Bioinformatics Facility, High Content Imaging Core, Cell Biology and Image Acquisition, Histology/Pathology Core
Funders: Canadian Institutes for Health Research
The Ottawa Hospital is a leading academic health, research and learning hospital proudly affiliated with the University of Ottawa.
